In this blog series, we examine the differences between activities of daily living (ADLs) and instrumental activities of daily living (IADLs), and what happens when they become difficult for a person.
In part one of our blog series “ADLs vs. IADLs,” we discussed activities of daily living (ADLs) — essential self-care tasks, like bathing and dressing, needed to live independently. Assessing a person’s ability to perform ADLs provides a clear picture of their functional status and can help determine when support and/or care services are needed. But what are the options when some or all ADLs become difficult for an older adult? And how can this impact the timing of a potential senior living move?
Three common paths when ADLs become challenging
When issues with independently, safely, and effectively performing one or more ADLs arise and persist for an older adult, there are typically three paths to consider:
- Can an unpaid/family caregiver plus certain home adaptations support still safely living independently?
and/or - Does a paid in-home caregiver need to be hired?
or - Is it wiser/safer to move to an environment where personal care services are built in, such as an assisted living community?
Let’s take a closer look at each of these potential options for when ADLs become difficult for an older adult.
Using unpaid family caregivers
Many older adults initially turn to family (a spouse/partner, adult children, or other relatives) to help when some level of ADL support is needed. Benefits of this approach include staying in the same home, being cared for by familiar people, and cost-savings. But there are also potential drawbacks that come with this option:
- Stress: Family caregivers often experience a heavy emotional and physical toll, especially when assisting with personal care (like bathing and toileting), as well as a potential financial burden from lost time at work and lost savings for their own retirement years.
- Availability: If the unpaid caregiver’s health, availability, or willingness to assist declines, alternate arrangements can be difficult to coordinate.
- Unexpected costs: The older person’s home may increasingly require difficult or costly modifications (grab bars, stair lifts, bath seats, etc.) in order to remain a viable and safe living environment.
While staying at home with family support may work for a while, it’s important to ask: How sustainable is this over the long term, and what happens if, for whatever reason, the unpaid caregiver is no longer available?
>> Related: Family Caregiving Can Present an Array of Stressful Challenges
Hiring paid in-home caregivers
If unpaid caregivers are not an option or need backup, hiring a professional home care provider (aka, personal care aide or home care aide) is a common next step for those who need help with ADLs. The advantages: You remain in your home, and help can be scheduled for specific tasks (e.g., help with bathing, dressing, toileting, meal prep, transfers, etc.). But there are tradeoffs to using paid caregivers as well:
- Cost: Ongoing paid help can become expensive quickly — averaging over $6,400 per month for just 44 hours of assistance each week. (The CareScout/Genworth Cost of Care Calculator shows what you might expect to pay for care in your area.) And what’s more, most of those in-home, non-medical long-term care costs are not covered by Medicare or health insurance plans, meaning the expense will be out-of-pocket for the care recipient and/or their loved ones.
- Scheduling: In many regions of the U.S., there is a shortage of qualified home health aides as well as variability in quality. As a result, scheduling can be challenging and care can be inconsistent.
- Oversight: Someone (often a loved one) must still coordinate the care, monitor quality, and be present for supervision or back-up if the paid caregiver fails to show up.
For those who want to age in place in their current home, paid in-home care may be the right choice when ADL needs are moderate and stable, and necessary home modifications are manageable. But when ADL needs escalate or require significant assistance and supervision, or if healthcare services are also needed, the home environment plus paid home care provider option may become less efficient, less safe, and possibly cost-prohibitive.
>> Related: What is a Home Care Provider?
Moving to an assisted living community
When difficulties with ADLs become frequent, complex, or unpredictable, transitioning to a retirement community setting that offers personal care services often makes sense. An assisted living community is a type of long-term care facility specifically tailored for older adults who need non-medical support services, such as help with ADLs. Benefits of moving to an assisted living community include:
- Built-in personal care assistance and often 24-hour supervision, eliminating the need for assistance from unpaid family caregivers, and alleviating the stress of coordinating paid in-home caregivers
- Integrated social engagement opportunities, meals, and transportation, reducing the burden that daily life can impose as physical ability declines
- Peace of mind for the older adult and their loved ones because the community is structured for these specific care needs
However, moving into an assisted living setting can present its own set of hurdles. For one, it requires touring multiple communities and financial planning to cover monthly fees, which aren’t usually covered by Medicare/insurance. (Again, the CareScout/Genworth Cost of Care Calculator shows what assisted living costs in your area.) But perhaps more difficult, it means admitting you need support and moving out of an often-beloved home, both of which can be psychologically difficult for some people to swallow.
>> Related: The Cost of Assisted Living: What You Need to Know
A brief note on proactive senior living moves
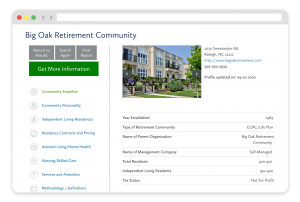
For those who wish to proactively plan for any future care needs, a move to a continuing care retirement community (CCRC, also called a life plan community) while you are still independent and relatively healthy may be a solution. CCRCs include independent living residences, as well as providing residents with access to assisted living and skilled nursing care as their needs evolve.
A proactive move to a CCRC can offer peace of mind, providing access to whatever level of care you may eventually require while also reducing the risk that a sudden health crisis necessitates difficult caregiver decisions and/or forces a relocation.
But it’s important to know that in order to qualify for certain CCRC contracts, you must be healthy enough to pass the community’s health assessment, so if assistance with ADLs is already needed, a CCRC may or may not be a viable option.
>> Related: Understanding the CCRC Health Evaluation Requirement: When Is the Right Time to Move?
Thinking through the right time for a senior living move
For those considering a senior living move, one of the biggest questions often is: “When is the right time to move?” The answer is usually: ideally, before a health crisis forces the decision.
Here are some practical questions to ask yourself (and perhaps discuss with your loved ones and financial advisor) when considering the timing of a senior living move.
- How many ADLs do I currently perform completely on my own vs. how many require some level of assistance, supervision, or extra effort? (It can be helpful to actually list each of them: bathing, dressing, toileting, transferring, eating, walking.)
- Have I had recent episodes of falls, near-falls, and/or hospitalizations, or am I having increasing difficulty with mobility or transfers?
- Could my home environment be modified to remain safe (bathroom grab bars, no steps, adequate lighting, etc.), and am I emotionally and financially comfortable making those modifications?
- If planning to rely on family or other unpaid help: Are my loved ones willing and able to assist me indefinitely and as my care needs evolve? What is my backup plan if they can’t help?
- If considering paid help: Can I afford it indefinitely? Are there high-quality home care aides available locally? Am I able to coordinate and supervise care? Am I comfortable having someone I don’t know in my home?
- How important is it to me to avoid a sudden or forced move (for example, after a fall, hospitalization, or other health crisis)? Would being in a retirement community that offers residents access to personal care services if needed offer me peace of mind as a proactive step I can choose to take rather than a reactive one that is beyond my control?
- Have I toured at least two or three retirement communities to compare service levels, contract types, cost, level of care included, and how they serve residents whose ADL needs are becoming more demanding?
>> Related: When “What If” Happens: What to Do After a Health Crisis
Stay in control: Planning ahead, before ADL needs are urgent
Recognizing the early signs that assistance with ADLs may be needed often gives you more options: stay at home with unpaid family caregivers or paid help, or move into a retirement community designed for the changing needs that sometimes come with aging. For those considering a CCRC, planning ahead particularly matters since CCRCs often have health requirements in order to qualify for continuing care/lifecare contract-types.
Some older adults prefer to make a proactive senior living move when they are still relatively independent and have more choices, rather than waiting until a health crisis forces the decision under stressful circumstances. If this sounds like you, proactively touring retirement communities, reviewing their care services, comparing contract options, and talking with current residents can create a sense of empowerment as well as peace of mind.
In next week’s post, we will further discuss instrumental activities of daily living (IADLs).
FREE Detailed Profile Reports on CCRCs/Life Plan Communities
Search Communities






