In this blog series, we examine the differences between activities of daily living (ADLs) and instrumental activities of daily living (IADLs), and what happens when they become difficult for a person.
As we age, one of the key measures of a person’s ability to live independently is how well they can manage activities of daily living (also called ADLs). ADLs are the everyday tasks required to care for oneself and move safely through the day. Changes in a person’s ability to safely and/or satisfactorily perform ADLs often signal that it is time to consider additional support.
When thinking about whether to remain in your current home or proactively move into a retirement community where help is readily available if needed, it’s important to understand exactly what ADLs are and how they can impact your senior living options.
What are ADLs?
The term “activities of daily living” refers to the basic self-care tasks that most healthy adults perform each day without assistance … or even much thought. ADLs include things such as eating, dressing, bathing or showering, toileting and managing continence, transferring (for example, getting in and out of bed or a chair), and mobility (walking or moving around).
ADL tasks are considered a good barometer of how well someone is functioning on their own. However, when one or more ADL becomes difficult or unsafe for a person to perform, remaining truly independent at home becomes more challenging.
The difference between ADLs and IADLs
To draw a quick but important distinction: ADLs are the basic personal care tasks. Instrumental activities of daily living (IADLs), on the other hand, are the more complex activities needed to safely and healthfully live independently within the broader community. They include important tasks such as managing medications and finances, grocery shopping, driving or using public transportation, and housekeeping.
In some cases, IADLs may decline earlier, however a deterioration in the ability to perform ADLs is often a more critical trigger for moving from living independently to needing assisted living services. In part 3 of this blog series, we will further discuss IADLs.
Why the ability to perform ADLs impacts independent living
Being able to perform ADLs safely and reliably is foundational if you want to continue living in your home, whether alone or with minimal support. They matter for a number of reasons:
- Safety: There are several potential safety issues that can arise as it relates to ADLs. For instance, if you have trouble transferring in and out of bed or a chair, the risk of falls increases sharply. If bathing or toileting becomes difficult, the risk of skin problems, hygiene‐related infections, or accidents grows.
- Quality of life: Difficulty with ADLs can reduce a person’s quality of life. It can impact the ability to engage in daily routines, resulting in isolation. Trouble with ADLs also diminishes independence, often leading to greater reliance on others just to maintain basic dignity and comfort.
- Early warning sign: In many aging and long-term care studies, limitations with ADLs is used as a predictor for needing home care, moving to an assisted living or skilled nursing facility, and increased risk of hospitalization.
- Planning for future support: Knowing your current ADL status helps you and your family anticipate how much help you might need (and when). This could range from modest home adaptations and part-time paid or unpaid caregivers, to transitioning to a care setting with personal care built in.
>> Related: Aging at Home or in a Senior Living Community: The Freedom of Choice
When ADL difficulty begins impacting safety or living arrangements
Recognizing that a loved one’s (or your own) ability to perform ADLs is diminishing is key. Care decisions made early tend to go more smoothly than choices made under pressure or during a time of crisis. Some practical red flags that may signal that it’s time to seek care assistance include:
- Needing help or supervision to transfer safely in or out of bed or a chair and/or moving about the home has to be done carefully and slowly
- Bathing, grooming, and/or dressing take significantly more time and effort or pose a risk of falling/slipping
- Relying on someone else to assist with toileting, managing incontinence, or cleaning up after using the toilet
- Eating and self-feeding becoming more difficult; maybe the person can still eat but they cannot prepare food comfortably or they tire while eating
- Mobility or walking becoming limited (the person avoids going out, is confined more, or has had near-falls)
- Becoming increasingly dependent on others for IADL tasks (grocery shopping, paying bills, driving), which often coincides with worsening ADLs
>> Related: Considering The Push-Pull Factors of Senior Living Moves
The next steps when ADLs become a challenge
Your ability to perform ADLs is one of the most practical and meaningful measures of how well you can continue to safely live independently in your home. As difficulty with ADLs increases, so do risks, burdens, and the need for support (either unpaid or paid).
In the next post in this blog series, we will look at the options people have when performing their ADLs becomes difficult or unsafe, and how to decide on the ideal time to make a senior living move.
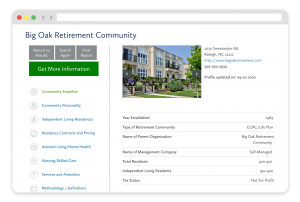
FREE Detailed Profile Reports on CCRCs/Life Plan Communities
Search Communities






