For many Americans, the happenings in Washington, D.C., might seem far-removed from their day-to-day lives. But as staff from numerous federal departments are eliminated, and our nation’s policymakers deliberate over significant budget changes and cuts, older Americans across the country stand to be profoundly impacted.
No matter which side of the political divide you stand on, it is important to understand how the policies in D.C. might end up impacting your life (and wallet) … or that of your loved ones.
Medicaid cuts would hit numerous older adults
The Medicaid program was authorized by Title XIX of the 1965 Social Security Act, signed into law by Lyndon B. Johnson. The program, which is jointly run by federal and state agencies, defrays medical costs for those with limited income and resources.
While many people think of Medicaid as helping low-income Americans, including children, it’s important to understand that it also serves as a critical lifeline for many older adults, particularly when it comes to funding long-term care (LTC) services.
In fact, Medicaid is the largest source of payment for long-term skilled nursing care in the U.S., covering more than 60% of nursing home residents, according to Centers for Medicare and Medicaid Services (CMS) and Kaiser Family Foundation data. These percentages are even higher in some of the nation’s poorest states.
One issue is that people are often surprised to learn that Medicare does not cover most long-term nursing home care, which averages $114,665 per year for a semi-private room, according to Genworth data. It’s easy to see how such an expense can quickly deplete an older adult’s savings thus requiring them to rely on Medicaid to pay for the care they require later in life.
This can even happen to those who were not previously low-income or destitute (and notably, some older adults even intentionally move assets out of their estate into Medicaid trusts in order to qualify for Medicaid). Therefore, all Americans, including older adults, need to understand the impact that Medicaid cuts could potentially have on their wallets.
>> Related: A Little-Known Detail about Medicaid Qualification and Paying for Long-Term Care
Even more nursing home closures
The proposed federal budget cuts to Medicaid — ranging from $700 to $880 billion over the next decade — could significantly disrupt a crucial safety net system. But the ripple effect of these cuts may be even wider spread than some people anticipate, even hitting older Americans who are financially secure but who require in-patient skilled nursing care.
Previous Medicaid cuts and financial strains have already led to the closure of a dramatic number of our nation’s nursing homes in the past decade. However, these most recently proposed budget cuts could lead to even more skilled nursing facilities closing due to decreased provider payments. Such closures will likely hit rural and poorer regions (where care options are more limited) particularly hard.
Future nursing home closures may also yield the perfect storm with lower supply and higher demand for skilled nursing care. As the Baby Boomers age, we expect to see a record number of people requiring long-term care services in the coming years. With fewer options for full-time/in-patient long-term care, numerous older Americans may be forced to endure substantial financial stress and emotional burden.
What’s more, a growing number of family members may be forced into unpaid caregiver roles as nursing home options continue to wane. This scenario can result not only in lost income for the unpaid family caregiver but also in sometimes overwhelming physical, emotional, and financial stress.
>> Related: The High Price of Family Caregiving
Reductions in Older Americans Act programs
Budget cuts may also necessitate reductions in eligibility and access to other types of care and services that many older people depend on. For instance, home- and community-based services (HCBS), which help older adults remain in their homes, are particularly vulnerable.
Although the Older Americans Act (OAA) funds many of these essential HCBS programs, recent budget proposals suggest eliminating or significantly reducing funding for many OAA programs since most of these programs are optional benefits, per federal law. According to an April report from the National Council on Aging (NCOA), some OAA initiatives being considered for reductions or elimination include:
- The Senior Community Service Employment Program (SCSEP): Proposed elimination could displace approximately 40,000 low-income older workers annually.
- Nutrition services: Cuts of $37 million threaten meal programs that serve millions of homebound older adults, many of whom rely on these meals as their primary daily nutrition.
- Fall prevention programs: Reducing funding for fall prevention could increase the risk of injuries among older adults, ultimately leading to higher healthcare costs.
Additionally, there is discussion in Washington that groups like the Administration for Community Living (ACL), which oversees a SHIIP- a critical consumer education program for older adults, as well as the Administration on Aging, and the Administration on Disability be reorganized or dissolved, with their programs moving to other U.S. Department of Health and Human Services (HHS) agencies — that is, if their funding is continued. This could result in even fewer supportive programs and services for our nation’s older population.
>> Related: Home- and Community-Based Services: An Increasingly Popular Care Option
Potential cuts to Veterans Administration services
The Veterans Health Administration (VHA) provides vital health services to millions of our nation’s veterans, a large percentage of whom are older adults. According to the U.S. Department of Veterans Affairs (VA) (PDF), as of 2023, more than 13 million veterans were eligible to receive care from the VA, and more than half of veterans enrolled in VA health care were age 65 or older.
But despite the growing number of older veterans, there are proposals within the federal budget to cut VA services or limit funding, which could lead to:
- Longer wait times for critical services, including geriatric care, rehabilitation, and mental health support.
- Closure or consolidation of VA medical centers, especially in rural areas where alternatives may be limited.
- Reduced availability of home-based primary care and extended care services, which are vital for many aging veterans with chronic health issues or mobility limitations.
Limiting these programs could jeopardize many older veterans’ ability to age with dignity, independence, and proper support — care they earned through their sacrifices for our nation.
Immigration policies and the caregiving workforce
There is yet another hot topic issue in Washington, D.C., that stands to impact the facility-based and home-based senior living and care industry across the country: the issue of immigration.
Once again, regardless of your political leanings, there is no denying our nation’s dependence on immigrant labor. This is perhaps particularly true in many lower-paying jobs such as care services, custodial and housekeeping services, and food service, all of which are integral to high-quality senior living, care, and support services. For example, approximately 40% of home health aides, 28% of personal care workers, and 21% of nursing assistants are foreign-born, according to Bureau of Labor Statistics data from 2022.
Proposed immigration crackdowns, including mass deportations and hardline restrictions on legal immigration, threaten to substantially deplete this vital workforce. Such shortages could lead to decreased access to care for older adults, poorer quality of care, increased workloads and stress for remaining staff, and overall higher costs for families … also, potentially forcing some loved ones to take on unpaid caregiver roles.
>> Related: The Crossroads of Immigration Reform and Long-Term Care
Understanding the big-picture impact of D.C. budget cuts
Again, putting politics aside, it is important for everyone to understand the potential impact of federal budget cuts and proposed legislative changes, and the significant challenges they may create for older adults nationwide and their loved ones. Not only might these budgetary measures reduce access to essential healthcare, support services, and caregiving resources, but they could also potentially diminish the quality of life of countless older Americans.
As these latest budget proposals advance through Congress, it is crucial to consider their far-reaching implications on our aging population and to engage in informed, civil discussions about the future of elder care in the U.S., both from a quality and affordability standpoint. We all owe that to our nation’s older generations.
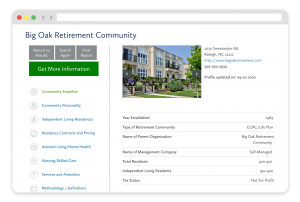
FREE Detailed Profile Reports on CCRCs/Life Plan Communities
Search Communities






