For fiscal year 2020, 76.5 million Americans were enrolled in Medicaid, including 6.4 million seniors. Medicaid is the single largest payer for long-term care in this country. In part, that’s because the cost of long-term care can be so exorbitant — averaging $51,600 a year for assisted living and $93,000 for a semi-private nursing home room (according to Genworth).
A large portion of Americans either underestimate how much such care will cost, or how long they will need it — or both. Others simply do not have the means to adequately save for retirement and those potential care costs. Medicaid has made it possible for these low-income seniors to age with dignity, accessing the care services they need, regardless of their ability to pay.
But how is Medicaid qualification determined? Could it be that, even if you own a number of assets (such as a home), you may still be eligible for Medicaid coverage?
>> Related: 4 Ways to Pay for Long-Term Care Services
Details around Medicaid qualification
Medicaid financial eligibility is determined by a complex equation that assesses a person’s income plus exempt and nonexempt assets. Exempt assets include things like one vehicle, your home/home equity (up to a certain dollar amount), cash up to $2,000, and a few other items. Nonexempt assets are basically anything else you own, and they must be used to contribute to the cost of your care before Medicaid will begin to pay.
Those so-called “exempt assets” can create some interesting situations when it comes to Medicaid eligibility, however. That’s in part because seniors in the United States hold in excess of $8.05 trillion of home equity. Medicaid exempts between $603,000 and $906,000 of a person’s home equity wealth when determining their financial eligibility for long-term care coverage, which is the program’s most expensive benefit. To some, this may seem like a lot for a program that is designed to be a safety net program.
Researchers at the University of Minnesota’s School of Public Health determined that a huge percentage of today’s seniors would be below the Medicaid home equity threshold, making them financially eligible for long-term care support services.
There are 54 million people in the U.S. who are age 65 or older, according to the latest Census data, and Harvard research has found that 78.7 percent of American seniors own their own home. That means that millions of seniors may be eligible to receive trillions of dollars in Medicaid long-term care benefits without having to expend their home equity.
A recent article in the New York Times described how baby boomers are holding onto their homes instead of selling, which is a contributing factor to the tight supply of home inventory. It’s reasonable to assume that some of these retirees are holding onto their largest asset in order to protect it from Medicaid. However, there is a little more to this…
>> Related: So I’ll Probably Need Long-Term Care, But for How Long?
Recouping Medicaid expenses
If it sounds like a lot of taxpayer money is being spent on long-term care costs for Medicaid recipients, it is, but the government does have ways to recover some of that expense.
The Omnibus Budget Reconciliation Act of 1993 (OBRA 93) required state Medicaid programs to recoup at least a portion of the cost of care from the estate of deceased recipients. This expense recovery does permit the state to tap into the decedent’s home equity.
In essence, this means Medicaid is not “free money.” It operates more like a government-backed loan program, which must be repaid when the recipient dies, assuming a qualified surviving dependent does not need the money or asset.
Medicaid qualification with a Medicaid trust
A Medicaid trust, also called a Medicaid qualifying trust, is an irrevocable trust that can potentially help someone in need of long-term care qualify for Medicaid while protecting certain assets from being counted in the Medicaid financial eligibility formula (which, again, factors in a person’s exempt and nonexempt assets).
In short, by transferring their assets into a Medicaid trust, a person is no longer considered the owner of the asset and relinquishes control over how the money is used. Instead, a designated trustee is legally responsible to ensure the funds are managed and used in accordance with the terms of the trust. But again, remember that all of this is applicable only for Medicare-/Medicaid-certified facilities — not self-pay facilities.
There are some ethical considerations around the use of Medicaid trusts. Creating such a trust with the primary objective of using government assets (a.k.a., taxpayer money) to pay for your care, instead of paying for it with your own money, is considered by some to be morally dubious. Many would argue that this method of engineering Medicaid eligibility should only come as a supplement to other legitimate retirement planning — not as a way to simply avoid paying for one’s own care.
It’s also important to know that any transfer of assets — whether to a family member, a charity, or even a trust — will be subject to a five-year look back period. If the transfer was made within five years of a person’s application for Medicaid, then a penalty period will be assessed during which the applicant will not be eligible for Medicaid benefits. The larger the amount of assets given away or put in a trust, the longer the penalty period.
(As a side note, a similar look back policy often applies to continuing care retirement communities [CCRCs, also called life plan communities] should a resident run out of money.)
>> Related: Medicaid Trusts and Continuing Care Retirement Communities
Medicare vs. Medicaid for long-term care costs
It is vital for seniors to understand what long-term care expenses are and are not covered by Medicare and Medicaid.
For example, Medicare does not cover long-term care costs for assistance with activities of daily living (ADLs) if that is the only type of care required by the senior. In other words, Medicare typically doesn’t cover the types of services provided in an assisted living facility. It will cover some of the cost of skilled nursing care, however, which includes medically necessary needs such as wound care, IVs, and drug administration.
Medicaid, on the other hand, will typically cover the cost of assisted living services, as well as skilled nursing care, for those who qualify financially. But bear in mind: For both Medicare and Medicaid, services must be delivered by a Medicare-/Medicaid-certified provider in order to be covered at all. Otherwise, all costs will be self-pay, i.e., out of the care recipient’s pocket.
>> Related: Long-Term Care: How Much Does Medicare Actually Cover?
Meeting a growing demand for long-term care
Access to long-term care services, ranging from help with one or two activities of daily living all the way up to full-time skilled nursing care, is a steadily growing need in this country. The U.S. Department of Health and Human Services (DHHS) estimates that somewhere between 50 and 70 percent of people over the age of 65 will require fairly significant long-term care services at some point in their lifetime.
Finding the human resources needed to fulfill this ever-increasing demand is an ongoing issue, but for many seniors, affording the care services they require is even more daunting. The Medicare and Medicaid programs can potentially alleviate some of this financial strain, but as a country and a society, we need to do more to support seniors so they can receive the care they need to age with dignity.
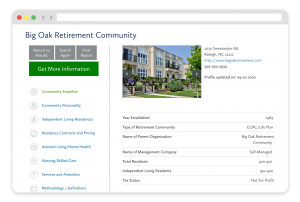
FREE Detailed Profile Reports on CCRCs/Life Plan Communities
Search Communities






