When family caregivers and home health care providers are no longer able to meet a person’s care needs, some families make the decision to move their loved one to a skilled nursing facility, also called a nursing home. It’s important to understand the potential costs of long-term care in a nursing home as well as how billing and contracts work for the average nursing home stay.
What is a nursing home?
A nursing home, also called a skilled nursing facility, is a type of long-term care residential community that provides higher-level medical care and supportive services for residents. According to the most recent comprehensive stats from the CDC’s National Center for Health Statistics National Study of Long-Term Care Providers (NSLTCP) (2018 data), there are approximately 1.7 million beds in 15,600 nursing homes in the United States, 70% of which operate as for-profit businesses.
As compared to an assisted living community, where residents may just need help with a few activities of daily living like dressing or bathing, nursing home residents usually require 24-hour monitoring and medical assistance.
The care provided at a nursing home is usually not as intensive or comprehensive as what a patient might receive in a hospital setting, however. There will usually be a physician overseeing the facility, but most day-to-day care at a nursing home is provided by nurses (RNs, LPNs), health aides, or specialized therapists (e.g., occupational, physical, or speech pathology).
>> Related: What’s the Difference Between Assisted Living and Nursing Care?
How long is the average nursing home stay?
Some nursing home residents are only there for a limited time to receive short-term rehabilitation care following a hospitalization, serious accident, surgery, or illness. Other residents require the type of skilled nursing care provided by a nursing home indefinitely.
The NSLTCP’s most-recent data (2022 report, Appendix III, Table XIII with 2018 data) states that the average stay in a nursing home is 485 days, but keep in mind that’s an average. Approximately 43% of nursing home residents are short-stay — spending under 100 days in the facility’s care. Again, this may be the case for people who need post-surgical care or who need rehabilitative services following a serious medical event like a stroke or heart attack.
The other 57% of nursing home residents are considered “long-stay” patients, remaining in the care of the facility for over 100 days. These long-stay patients are usually older and more infirm, and over half (57.6%) suffer from some form of dementia — often alongside other comorbidities.
But it’s important to note that not all nursing home residents are elderly, with 16.9% of residents younger than age 65, according to NSLTCP. Again, these may be people who need a short-term stay after a surgery, or they may be people with severe developmental disabilities who need skilled care and are long-stay residents.
>> Related: The Emotional and Financial Cost of Dementia and Memory Care
Costs of long-term care
According to Genworth’s Cost of Care Survey, in 2023, the average monthly cost of a semi-private room in a nursing home is $8,390. A private room will run even higher, averaging $9,584 per month. If the average stay in a nursing home is 485 days, or around 16 months, that translates to over $134,240 for the semi-private room and $153,344 for the private one! (As an aside, 24-hour care in one’s own home would likely cost considerably more than this.)
But as with nearly everything, the costs of long-term care at a nursing home are creeping up each year. In just five years (2028), Genworth projects that a semi-private nursing home room will cost approximately $9,726 per month, and a private room will top $11,100 monthly.
Keep in mind: These are just averages. The cost may be higher or lower depending on where you live and the specific facility — as well as supply and demand, and the long-term rate of inflation.
>> Related: What Will My Long-Term Care Cost?
How to pay for long-term care at a nursing home
For most people, the six-figure cost of the average stay in a nursing home is pretty eye-popping. If you are worried about how to pay for long-term care in a nursing home, there are several things you should know…
Medicare and health insurance coverage
If a nursing home resident’s medical needs meet Medicare Part A’s “skilled medical care” criteria, as well as other specific requirements, and the facility is Medicare-certified, Medicare usually will pay in full for up to 20 days in a nursing home (though this is not guaranteed). For days 21-100, Medicare typically will continue to pay, but a variable rate daily coinsurance amount kicks in, which is the financial responsibility of the resident. Beyond 100 days, 100 percent of the charges become the responsibility of the resident. Learn more about Medicare’s criteria for paying for long-term care.
For residents with a secondary health insurance policy or a Medigap plan, on days 21-100, it may cover some or all of the balance of expenses not covered by Medicare. Be sure you understand the terms of your specific policy to ascertain if there is any coverage for skilled nursing care at a nursing home.
Long-term care insurance (LTCi) policies
The terms of LTCi policies can vary widely, so be sure you understand exactly what your/your loved one’s policy will and will not cover. Also, be sure to let the nursing home know if your loved one has an LTCi policy.
Most LTCi policies will make payments on the policy directly to the resident (i.e., the policyholder). Some will pay the nursing home directly, however, so if this is the case with your/your loved one’s policy, be sure to ask the nursing home’s billing office to send monthly invoices for nursing care services directly to the LTCi policy carrier. This will save time and frustration.
Any nursing home costs that are not paid by the LTCi policy become the resident’s financial responsibility. Also know that most LTCi policies do not cover the cost of any state taxes assessed on the bill.
Medicaid coverage
Medicaid is a government safety net program for people who no longer have the assets and income to pay for their own care. If a nursing home resident’s available assets dip to the point of having funds to cover only three more months of private payments for their care, they may become eligible for Medicaid.
Your county Department of Social Services can typically provide information on the requirements for filing for Medicaid. It can be a complex application process that takes 3+ months to complete. There is also a five-year “lookback” period during which Medicaid will verify you have not given away your assets. Learn more about the Medicaid lookback period.
Notify the nursing home’s social work department and/or billing office if and when you begin the application process, and keep them apprised of any status updates you receive. Some nursing homes even provide assistance with the application paperwork at no charge.
A few caveats about paying for care
It’s crucial to know that if you sign an agreement with a nursing home, that ultimately makes the resident or their proxy the responsible party for any payments due to the nursing home.
Most nursing homes would rather bill a private party (the resident or their proxy) than seek reimbursement from Medicare or Medicaid. In fact, some nursing homes only accept private payment, but many states prohibit this policy.
In rare cases, a state with filial law can compel a resident’s adult child to pay their parent’s bill, even if the child did not sign the resident agreement. If you feel that your loved one may need to move to a nursing home in the near future, it is wise to talk with an experienced elder care attorney before any documents or contracts are signed.
>> Related: The Pain of Paying for Long-Term Care is Real; A CCRC Can Help
How nursing home billing works
The frequency with which a nursing home bills a resident, or a resident’s proxy, will be spelled out in the terms of the resident contract. Most will send an invoice on a monthly basis and will be prorated if the resident was only there for part of the month.
The bill will include the basic residency charge plus charges for any ancillary services the patient received during the month. The billing rate also will be impacted by the complexity of the care required by the resident, level of services, whether it is private or semi-private room, and other amenities offered by the facility.
Oftentimes, a nursing home bill will include a “pre-bill” for the cost of the upcoming month, and depending on your state, there may be a tax on the subtotal of the bill. The amount owed by the resident (or their proxy) will be the balance of these figures after all payments from Medicare/Medicaid, health insurance, and/or long-term care insurance are deducted.
It’s important to note that this billing process may work slightly differently if your loved one is moving into the skilled healthcare center within a continuing care retirement community (CCRC, or life plan community), particularly if the person has a lifecare contract. Learn more CCRC contracts.
Shouldering long-term care costs
As more and more people are living longer, the need for skilled nursing care is going to become even greater. And as we discussed, the cost of the average stay in a nursing home can easily reach into the six-figures … and that cost is going nowhere but up. As a result, it is understandable that people are increasingly concerned that they might outlive their savings — potentially burdening their loved ones with the exorbitant costs of long-term care.
Residents of CCRCs may be able to avoid this concern, in some cases. Many CCRCs make a commitment to provide lifetime housing and care to their residents, even if a resident runs out of money and does not qualify for Medicaid or other assistance.
However, CCRCs also must look out for their financial viability to be sure they can keep their commitments to residents. As a result, CCRCs will do a thorough financial evaluation of new residents to help ensure that the probability of them running out of money remains low. Similar to Medicaid, a CCRC will typically do a five-year lookback if a resident runs out of money.
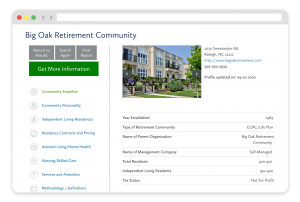
FREE Detailed Profile Reports on CCRCs/Life Plan Communities
Search Communities