In last week’s blog post, we shared how a home care provider’s assistance with activities of daily living (ADLs) can help older people remain in their home and independent for as long as possible. But we also shared that the cost of an in-home care provider is not typically covered by Medicare; it must be paid out-of-pocket by the care recipient or their family. Then this week, I read an article offering a real-life example of how Medicare classifies certain health conditions and their related long-term care costs to determine what they will and will not pay.
A real-world story about dementia and unpaid caregivers
This Huffington Post article was written by an adult daughter dealing with her parents’ declining health. Her father was diagnosed with Lewy body dementia about five years ago. Her mother served as his unpaid caregiver for several years until her mental and physical health began to deteriorate as well.
The family looked into an in-home care provider to help as the father gradually lost the ability to attend to his personal care needs like showering, dressing, and using the bathroom. They were shocked to find that the cost of assisted living services provided in the home would not be covered by Medicare.
The family eventually was forced to move the father into a memory care community to receive the care services he needed, which unpaid caregivers (family members) could no longer provide. With no long-term care insurance and dwindling retirement savings, this story of a middle-class family dealing with caregiving needs and the staggering cost of assisted living, and more specifically, the cost of memory care, is all too common.
>> Related: Special Considerations Surround Unpaid Dementia Caregiving
What care services Medicare will and won’t pay for
Medicare deems the care needed by those with dementia (which includes Alzheimer’s disease and many other degenerative memory conditions) as “custodial” or “companionship” and thus says the care can be provided by family members, i.e., unpaid caregivers. A Medicare representative put it in stark terms for the daughter who wrote the article: “We don’t consider dementia a medical issue.”
Now, if dementia were deemed a medical issue, Medicare perhaps would cover the cost of assisted living services needed to deal with certain aspects of the condition. As the article’s author notes, “If my father had cancer or heart disease, he would probably live at home with some home care covered by Medicare.”
And she is right. Regardless of whether provided in the home or in a communal setting, Medicare does not pay for non-medical assisted living services (i.e., custodial care or personal care) if that is the ONLY type of care needed. However, Medicare Part A will cover a limited amount of medically necessary skilled nursing care if certain requirements are met, such as:
- The care recipient must have first had an “admitted” hospital stay of three days or longer.
- Admittance into the skilled nursing facility must take place within 30 days of that hospital stay.
- A physician must state that daily medical nursing care or rehabilitation services are necessary.
- This care must be provided in a Medicare-certified facility. (Medically necessary services provided at home by a Medicare-certified home health care agency also may qualify.)
So, in most cases, skilled nursing care covered by Medicare follows a serious medical incident, like a stroke, heart attack, fall, or major surgery. Even though dementia is arguably a medical condition that impacts the brain, the type of supportive services needed on a daily basis are usually non-medical, and thus, the care needed for the father with dementia does not meet Medicare’s coverage criteria. (Visit Medicare.gov to learn more about what long-term care services are and are not covered.)
An important caveat: Medicaid, a government safety net program for those who no longer have the assets and income to pay for their own care, actually will cover some of the cost of assisted living services for those who qualify. Learn more about Medicaid qualification and what long-term care costs it covers.
>> Related: Long-Term Care: How Much Does Medicare Actually Cover?
The cost of assisted living
For some families like the one in the article, paid caregiving services become a necessity, even if it means paying out of pocket. So, how much is assisted living per month, and what if memory care is needed? As we discussed last week, the costs can vary greatly depending on how much care a person requires and where they receive it.
For example, according to Genworth’s Cost of Care Survey, in 2023 the average hourly cost of homemaker-type services from an in-home care provider is $27.58 per hour, or around $5,259 per month, for 44 hours of help each week. Again, in most cases, because this is not medically necessary care, Medicare would not pay this expense.
If medical-type services are needed, the cost of in-home care increases to an average $5,462 per month for 44 hours each week. However, because it may be deemed medically necessary care, Medicare may pay some or all of this cost if the in-home care provider is Medicare-certified.
Then there is the cost of care in a communal senior living setting. An assisted living community averages $4,774 per month for a private one-bedroom — a cost that is typically out-of-pocket for the care recipient and their family since the care is generally non-medical in nature.
For those who need a higher level of care, semi-private room in a skilled nursing facility (also called a nursing home) averages $8,390 a month, and a private room averages $9,584 each month, some or all of which may be covered by Medicare if it is medically necessary care.
Memory care, however, may have a higher price tag than these other types of long-term care services.
>> Related: What Will My Long-Term Care Cost?
The cost and average length of stay in memory care
Memory care is usually a special care unit within an assisted living community or skilled nursing facility (also called a nursing home) with advanced features to keep those with memory issues safe. They also have staff specially trained to care for those with dementia, and they may offer special therapeutic programs for their residents.
The average monthly cost for memory care can add another $1,000 to $4,000 a month to assisted living or skilled nursing care prices with some or all of this cost being out-of-pocket depending on the medical needs of the care recipient. So, with that, you could be looking at nearly $100,000 a year for memory care, with that figure being even higher in certain regions, facilities, and circumstances.
The average length of stay in memory care can vary greatly as well — from just a few months to several years — so the total cost of memory care could easily reach into the hundreds of thousands of dollars. (Here is a helpful life expectancy calculator for Alzheimer’s disease and dementia developed by Dementia Care Central with funding from the National Institute on Aging.)
>> Related: The Benefits of Customized Care in Special Care Units
Paying the price of dementia
As you can see, the cost of caring for a loved one with dementia can be staggering. It is understandable that most middle-class families, like the one featured in the Huffington Post article, would struggle to pay these costs, most of which are out-of-pocket since Medicare does not consider dementia to be a “medical issue.”
At the end of the day, many of the conditions that necessitate non-medical assisted living care are actually medically driven. Consider age-related health conditions like osteoarthritis that has created physical limitations. But to me, the stance by Medicare that dementia is not a medical issue and memory care is not medically necessary is difficult to stomach, particularly for anyone who has had to slowly say goodbye to a loved one suffering from this terrible condition.
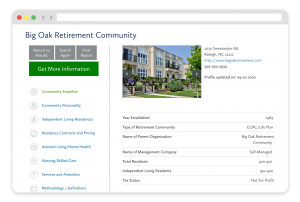
FREE Detailed Profile Reports on CCRCs/Life Plan Communities
Search Communities






