Senior care centers are generally considered to be assisted living facilities, memory care centers, or nursing homes. These senior care centers may be stand-alone facilities or operate as part of a continuing care retirement community (CCRC, or life plan community), which offers services spanning the entire continuum of care, ranging from independent living and including assisted living, memory care, and/or skilled nursing care. CCRCs provide a contractual promise to provide lifetime housing and care for their residents. A source of confusion for seniors or families researching a senior care center is understanding the difference between a “Medicare-certified” facility and a “private-pay” facility.
Simply put, a Medicare-certified senior care center accepts Medicare from patients and has met Medicare’s minimum requirements for patient care and management, including administration, clinical services, standards of excellence, and more.
Where Does Medicare-Certified Apply?
Medicare certification is only applicable to skilled nursing facilities(SNFs) – aka nursing homes- which are licensed in their respective state to offer 24-hour medical care provided by a registered nurse or rehabilitative staff, including procedures such as IV and drug administration, wound care, lab tests, physical therapy, and more. Therefore, if a CCRC describes itself as Medicare-certified it is likely referring to the skilled nursing unit within the CCRC. Such certification, or lack thereof, has no bearing on independent living centers or assisted living facilities because they do no provide skilled medical services.
People are sometimes shocked when they discover that a senior care center is not Medicare-certifed but the financial impact may be less than initially feared. Naturally, the term “private-pay” might lead a person to think the cost of care would be significantly more than the same it would for the same amount of care in a Medicare-certified facility. To better understand the true financial impact of recieving care in a private pay health care facility compared to a Medicare-certified facility it is important to first understand what Medicare actually covers.
Contrary to what many believe Medicare does not cover custodial care (assisted living or personal care) if that is the only type of care needed. However, Medicare[Part A] will cover the cost of skilled care provided by a Medicare-certified facility, on a limited basis. Generally speaking, your care must be preceded by a 3-day minimum hospital stay and Medicare will only cover costs associated with a semi-private room. The full cost of care under this scenario is covered by Mediare only for the first 20 days. Between 21 and 100 days Medicare will pay $148 per day (for the year 2013). After 100 days Medicare ceases to provide coverage. For more details visit: https://www.medicare.gov/coverage/skilled-nursing-facility-care.html
Here is a helpful chart that reveals an example of your maximum exposure in a private-pay facility compared to a Medicare-certified facility:
|
|
Medicare-Certified Facility |
Private Pay Facility |
Difference |
Total Days |
Total Difference b/w Medicare Certified and Private-Pay |
|
Days 1-20 |
$0 |
$220 |
$220 |
20 days |
$4,400 |
|
Days 21-100 |
$157.50 |
$220 |
$62.50 |
80 days |
$5,000 |
|
|
|
|
|
|
$9,000 |
National average daily cost of semi-private room in a skilled nursing facility. 2015 Genworth Cost of Care Survey.
Note: It is conceivable that the difference could be more than shown on this chart if you enter the skilled nursing facility more than once or if you were to choose a private-room instead of a semi-private room in the private-pay facility.
The above chart reveals the maximum out of pocket cost difference a resident would face over the first 100 days of care in a private pay senior care center compared to a medicare-certified senior care center. There is no guarantee that Medicare will cover up to the maximum amounts shown. In that case the cost difference would be even less. After 100 days Medicare ceases to provide any coverage, expect in the case of a re-admittance after a certain period of time has passed. Therefore, after 100 days a resident of the senior care center would pay for their care out of pocket regardless of whether they are receiving services in a Medicare-certified facility or a private-pay facility.
Learn more abour senior care centers and continuing care retirement communities.
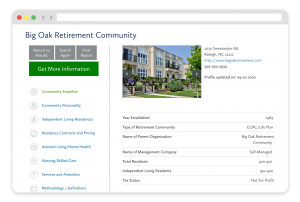
FREE Detailed Profile Reports on CCRCs/Life Plan Communities
Search Communities





