We see headlines all too often about the growing opioid epidemic in the U.S. and the skyrocketing number of fentanyl deaths. Recent data from the CDC shows that, among Americans aged 18 to 45, unintentional drug overdose is now the leading cause of death, above car accidents and suicide. But there is another “invisible epidemic” ravaging our country as well, and that is the growing incidence of substance abuse among older adults.
The increasing health effects of long-time habits
The Baby Boomers came of age in a time when attitudes about drug and alcohol use were shifting. What was once behavior to hide in the shadows entered the mainstream as substances like marijuana and psychedelic drugs became part of the youth “hippie” culture of the 1960s and 70s.
But as the Baby Boomers have gotten older, the drug and alcohol habits they formed in their youth have lingered for some. Now that they are in their 60s and up, these behaviors are having an increasing impact on older adults.
Physicians are increasingly seeing older adult patients with heart issues, cancer, liver and kidney disease, and cognitive impairment/decline being exacerbated by the patient’s substance abuse.
For instance, those who have been drinking regularly for many decades may now be facing liver damage or cancer caused by their alcohol use. Doctors are seeing a variety of cancers and cognitive issues among long-time marijuana smokers. And those who have often utilized opioids or amphetamines may have cardiovascular and neurological issues as well as an array of other health concerns.
This is all on top of concerns like prescription drug interactions, falls and other accidents caused by impairment, or even accidental overdoses.
>> Related: Higher Ed: Marijuana Use Increasing Among Seniors
Substance abuse among older adults is increasing
Beyond status quo use, research shows that drug and alcohol use among older adults is actually going up.
For example, in 2020, researchers out of the University at Albany analyzed data from the 2013–2018 Centers for Medicare & Medicaid Services Master Beneficiary Summary Files. They found that in that five-year span, estimated rates of opioid use disorder (OUD) among older adults in the U.S. increased more than threefold. OUD was particularly common among the so-called “young-old” — those 65–69 years old.
Alcohol use also has increased among older Americans in recent years, particularly during the COVID-19 pandemic. Studies out of Johns Hopkins and Columbia University found that drinking among all age groups increased during COVID, but the increase was most notable among people 65 and older, perhaps in part due to their increased risk for social isolation during that time. The 2022 National Survey on Drug Use and Health also found frequent binge drinking among approximately 20% of adults 60-64 years old and 10% of those over age 65.
Another 2022 study analyzed the overall incidence of substance use disorders among older Americans. The researchers found that 8% of Medicare beneficiaries under age 65 and 2% age 65 and older reported having some type of substance use disorder. Overall, among those reporting a substance use disorder:
- 77% had an alcohol use condition
- 16% had a prescription drug use condition (including opioid pain medications, tranquilizers, and anti-anxiety medications)
- 10% had a marijuana use condition
>> Related: A Hidden Pandemic Toll: The Rise in Alcohol-Related Deaths
Broader health implications of substance abuse among older adults
It’s important to keep in mind that the figures on older adults’ substance use/abuse derived by researchers may actually be much higher. While social norms about drug and alcohol use are evolving, there is often still a stigma around accurately reporting drug and alcohol use to physicians and researchers.
This underreporting of substance use can create even more issues for some older adults. For example:
- Healthcare providers may not be able to accurately diagnose the cause of certain common age-related symptoms a person may be having. What might appear to be cognitive decline could actually be the effects of opioid use. A balance issue or depression symptoms may really be the result of alcohol use. Stimulant use, on the other hand, may be mistaken for insomnia, anxiety, or certain heart conditions.
- Doctors run the risk of prescribing a medication that could interact with the other substances a patient is using, or cause an accidental overdose. For example, if a person is already using an opioid and the doctor unknowingly prescribes another pain medication, there is a risk of overdose. Alcohol can interfere with prescriptions like antibiotics, muscle relaxants, blood thinners (e.g., warfarin), and more.
- As people get older, changes naturally occur to the brain and body. These changes can make older adults increasingly sensitive to the effects of drugs and alcohol. This lower tolerance can raise their risk of interactions, accidents, or even overdoses.
>> Related: The Key Difference Between Social Isolation & Loneliness
A problem that retirement communities can help address
A sometimes-overlooked aspect of older adults’ substance use pertains to the implications for the senior living industry. A few considerations come to mind.
First, retirement communities should be cognizant of the safety-related issues surrounding their residents’ substance use. Older adults who are using drugs and alcohol may be more prone to accidents like slips and falls, as well as drowning or motor vehicle accidents. Appropriate safety measures — such as non-slip surfaces, safety lighting, and pool alarms — should be put in place to protect residents.
Next, there are various implications to the finances of a retirement community should a resident suffer a preventable injury or death as the result of substance use. There are of course concerns about adequate liability insurance coverage for the community, but there can also be reputational risk.
Continuing care retirement communities (CCRCs or life plan communities) can have an added cost associated with residents’ substance use. For those CCRCs offering life care contracts, the community will incur the long-term care costs associated with any health issues or accidents caused by a resident’s drug and alcohol use.
For these and other reasons, senior living providers should consider ways they can proactively address the growing incidence of drug and alcohol use among older adults. This might come in the form of offering on-site support groups for residents struggling with addiction. It also might include adding safety measures like ensuring ready availability of Narcan for opioid and fentanyl overdoses.
Perhaps one of the most important ways that retirement communities can help combat substance abuse among older adults is to continue their focus on providing numerous opportunities for social interaction among residents. Such social opportunities help nurture supportive relationships, which can in turn help a resident who might be struggling with drugs or alcohol, or might deter a person from turning to substances in the first place as a coping mechanism for loneliness, anxiety, depression, or grief.
>> Related: Suicide Among Seniors: An All-Too-Common Tragedy
Balancing therapeutic uses with health and safety concerns
It’s worth noting that there is some recent research into successful therapeutic uses of alcohol and some drugs that have traditionally been considered recreational or “party drugs.”
- For instance, just one dose of LSD (sometimes called “acid”) administered in a therapeutic setting has been shown to treat generalized anxiety disorder, thus receiving the FDA’s breakthrough therapy designation.
- Similarly, one or two therapeutic doses of psilocybin, the psychedelic in so-called “magic mushrooms,” can give lasting relief to people suffering from PTSD, major depressive disorder, anxiety, obsessive-compulsive disorder, and more.
- Ongoing research has found various therapeutic benefits associated with medical cannabis (marijuana) use, such as reductions in anxiety, insomnia, chronic pain, chemotherapy-induced nausea and vomiting, and spasticity associated with multiple sclerosis (MS).
- Resveratrol, a polyphenol found in red wine, may have anti-inflammatory and antioxidant properties when consumed in moderation, which some studies have shown may reduce the risk of cancer, lower blood pressure, and reduce plaque buildup in arteries and brain cells.
But despite these potential medical uses of alcohol and traditionally recreational drugs, we cannot ignore the increasing incidence of substance abuse and addiction among older adults in the U.S. The senior living industry, as well as society as a whole, must look for solutions to stem this growing “invisible epidemic” and help safeguard older adults’ health and safety.
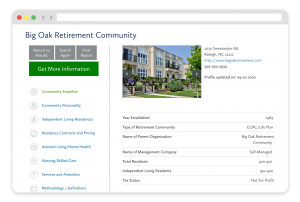
FREE Detailed Profile Reports on CCRCs/Life Plan Communities
Search Communities






